The Road to Health Equity Must Encompass a Strategy for Equitable Digital Health
In this interview with Edmondo Robinson, MD, Chief Digital Officer, Moffitt Cancer Center, he discusses how his hospital is applying a health equity lens to their digital strategy.
The COVID-19 pandemic proved how important technology is for keeping us connected. Telehealth visits and video calls kept isolation at bay and care continuing. Yet, because of institutional and structural issues, many people from historically marginalized communities continue to lack access to the internet or the skills to fully engage with digital health tools, such as patient portals, apps and telehealth platforms. Designing health technology to meet the needs of these individuals is a fundamental pathway to improve health equity. Yet discussions around health equity rarely focus on technology, while discussions around health technology rarely focus on equity. As digital health continues to expand, health care organizations must include a digital health equity strategy to ensure that all in their communities can access needed medical and social services.
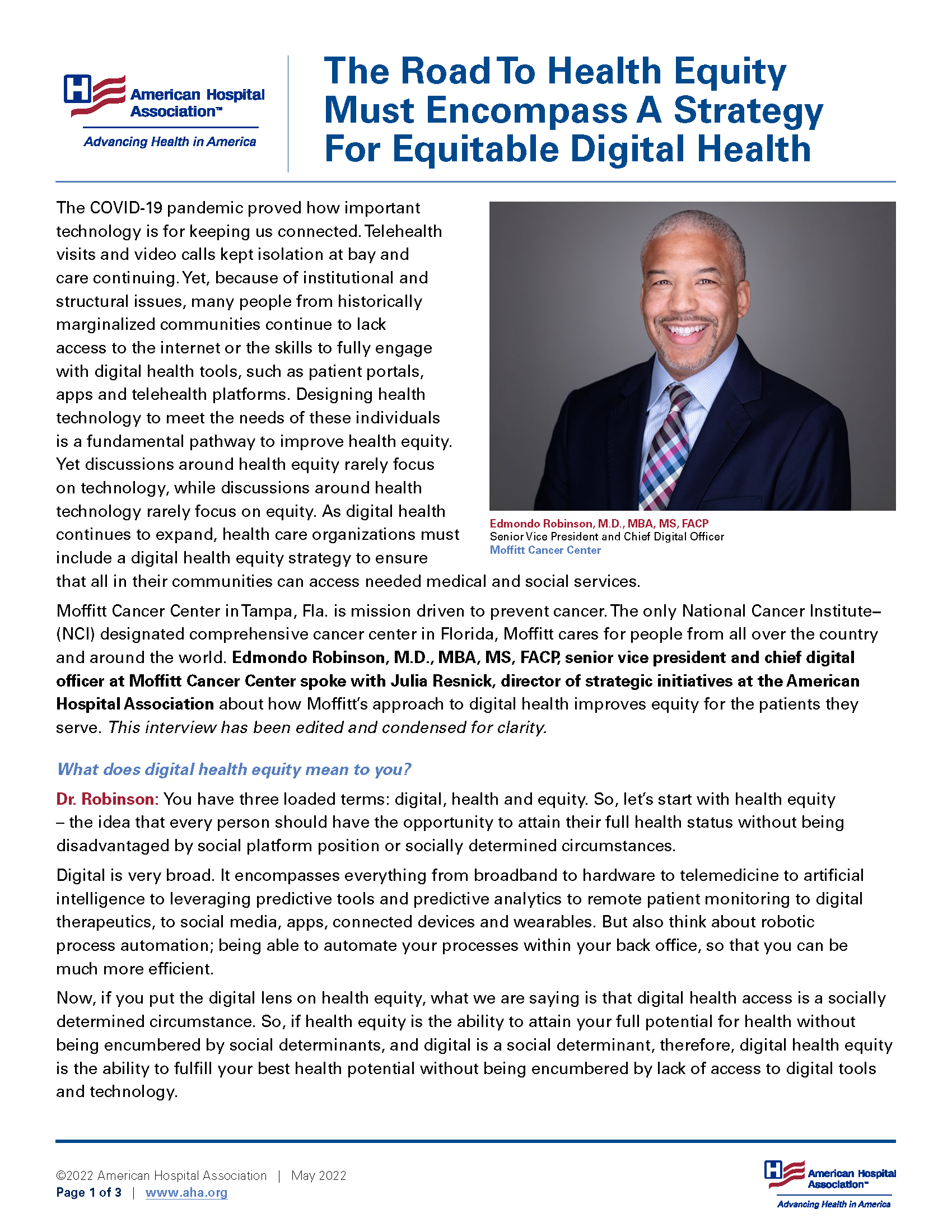
Edmondo Robinson, M.D., MBA, MS, FACP
Senior Vice President and Chief Digital Officer
Moffitt Cancer Center
Moffitt Cancer Center in Tampa, Florida, is mission driven to prevent cancer. The only National Cancer Institute (NCI) designated comprehensive cancer center in Florida, Moffitt cares for people from all over the country and around the world. Edmondo Robinson, M.D., MBA, MS, FACP, senior vice president and chief digital officer at Moffitt Cancer Center spoke with Julia Resnick, director of strategic initiatives at the American Hospital Association about how Moffitt’s approach to digital health improves equity for the patients they serve. This interview has been edited and condensed for clarity.
What does digital health equity mean to you?
Dr. Robinson: You have three loaded terms: digital, health and equity. So, let’s start with health equity – the idea that every person should have the opportunity to attain their full health status without being disadvantaged by social platform position or socially determined circumstances.
Digital is very broad. It encompasses everything from broadband to hardware to telemedicine to artificial intelligence to leveraging predictive tools and predictive analytics to remote patient monitoring to digital therapeutics, to social media, apps, connected devices and wearables. But also think about robotic process automation; being able to automate your processes within your back office, so that you can be much more efficient.
Now, if you put the digital lens on health equity, what we are saying is that digital health access is a socially determined circumstance. So, if health equity is the ability to attain your full potential for health without being encumbered by social determinants, and digital is a social determinant, therefore, digital health equity is the ability to fulfill your best health potential without being encumbered by lack of access to digital tools and technology.
Why is digital health equity a priority for Moffitt?
Dr. Robinson: As part of Moffitt’s mission, our job is to present cutting-edge treatments in the quest to prevent and cure cancer; digital is increasingly going to be a tool in the toolbox to get there. We must leverage digital as a core tool for all those that we care for − not just for people who have money, who have insurance or jobs. That means that equity is core to our mission and values − to make sure that we are reaching all of those that need our services.
What is Moffitt’s Center for Digital Health?
Dr. Robinson: The Center for Digital Health is a unique structure for a health care provider, certainly in the cancer center space. We are creating a structure around technology to support the entire enterprise. And we do not have a separate digital strategy. Our approach is to develop an enterprise-wide strategy that leverages and is enabled by digital. For example, the more efficient we are in a back office by leveraging digital technology, the more we can focus on direct clinical care and research.
The Center for Digital Health has three complementary departments. The core is the information technology (IT) department, led by our chief information officer, and contains all the elements that comprise a typical IT department in a health system, including cybersecurity, application support and infrastructure. The other two areas are a bit more unique. One is health data services, which is led by our chief data officer who is focused on using data as a tool to drive discovery, clinical care and optimal business processes. The third is the digital innovation department where we focus on ideating and creating the technology assets of the future – thinking about everything from the consumer voice and their needs to robotic process automation and remote patient monitoring. Those three departments work interdependently to drive the Center for Digital Health.
How is the Center driving digital health equity?
Dr. Robinson: We've been focused on digital access because access is a core component of digital equity. That may mean access to broadband, hardware, knowledge and more. Additionally, digital literacy is an important concept. There is also a design component in making digital tools equitable – everything from language translation options to font size for the visually impaired. It is increasingly important to bake equity into the design of digital tools.
Something else we are exploring is how we can use digital tools to decrease some of the disparities that we have in health care delivery. For example, as an NCI-designated comprehensive cancer center, we do a significant amount of research, including clinical trials. But can we explore an opportunity to increase the diversity of the clinical trial participants by leveraging an AI clinical trials matching tool?
A recent project with our Center was the use of digital tools for engagement and outreach. It was a quick 2-3 week pilot project focused on breast cancer screening in predominantly African American communities where women are disproportionately affected by breast cancer. By leveraging digital tools, we were able to increase our engagement by about 25 times and we developed 10 times as many partnerships as we would have otherwise been able to. We've projected that we could possibly increase our screening by 1,300 women based on the work from this pilot project alone. That's the power of the digital tools if you really leverage them to focus on equity.
What do you think that hospitals across the country can do on digital health equity and what is their role in this space?
Dr. Robinson: First you just need to identify that digital health equity is an issue. You have to acknowledge that 1) digital is important and 2) that equity is important. If your hospital has not identified equity as a core component of what you do, then you've got to start there. And if your hospital hasn’t identified digital as a core tool that you're going to leverage moving forward then you must go there as well. So, if digital is important and equity is important, then digital equity should be equally important. The next step is what you are going to do about it. Inclusion of digital health equity in your strategic planning is critically important. It seems like a simple first step, but it serves as a prerequisite for any future activities.
How do you make the case to health care leaders that digital health equity is a worthwhile investment?
Dr. Robinson: Because of the equity piece, much of this work is mission driven. But there are two scenarios at play: one where you don't want to be behind and there is one where you could be ahead. If you have not started to develop a strategy that leverages digital you're going to be behind. But the other case is if you become really good at digital, you're going to be more efficient and effective. And as you are managing populations and taking on risk, if you want to manage larger populations you need to leverage digital tools that you can scale with much more efficiency. You are going to improve your quality, your engagement, your outreach – and ultimately you will improve equity.
What are your recommendations for health care leaders who want to get started in digital health equity?
Dr. Robinson: I think it goes back to this idea of having strategies around digital and health equity. I'm going make an assumption that health equity is somewhere in your mission. You absolutely cannot assume that the digital folks know anything about health equity, especially if you bring them in from outside of health care. On the other side, the health equity experts may not know much about digital. That bi-directional learning can be very powerful.
This work requires leadership and investment in the people, tools, technology and infrastructure to build a digital core. Once you have your leadership and your investments in digital, you need to make sure that your mission-driven focus on health equity is baked into the digital aspects that you're building out. Then you hold your digital leadership accountable to that mission around health equity. Organizations that proclaim the importance of digital but do not have an identified digital senior leader are just talking, they aren’t doing.
Any parting words of wisdom?
Dr. Robinson: The time to start is now. Go for it. We are all trying to build the plane in the air. There might be some stumbles along the way, but we need to understand how to learn from those failures so that we improve over time. Being overly risk averse in digital holds us back from setting high goals and innovating. Understanding how to fail in digital is going to be an important skill for hospitals to advance their digital health equity strategies.
More AHA resources about digital health equity are available at www.aha.org/digitalequity.
For health equity resources, explore the Health Equity Roadmap at www.equity.aha.org and the Societal Factors Framework at www.aha.org/societalfactors.