
Population Health
Building Hospital-Community Partnerships
Leveraging strengths to improve community health
By Erica M. Osborne and Cindy Fineran
At the heart of most hospitals’ and health systems’ mission is the commitment to improve the health of the communities they serve. In recent years, there has been increased recognition of the immense impact that social determinants, or social needs, have on health – determinants that are wide ranging, complex and beyond the reach of a single health care organization.
It is well documented that unequal access to basic social needs such as housing, nutritious foods, employment and education all negatively affect health and life expectancy. Although hospitals are ideally positioned to provide clinical treatment to those who seek care in their facilities, the scope and multifaceted approach necessary to improve overall health is not a task that can be undertaken by one entity or one sector. To move the needle on community health, hospitals and health system boards are recognizing the importance of aligning their organizational efforts and partnering with others in their communities.
Speaking from the perspective of a community nonprofit that has partnered with hospitals and health systems, Kitty Bailey, executive director of Be There San Diego, an initiative to prevent heart attacks and strokes, observed that “hospitals and health systems that are truly mission driven and want to be good stewards of health and wellness for all recognize that they can’t do it alone.” She explained, “Their leaders are recognizing there are others in the community who have the expertise, experience and relationships that are critical to reaching people or populations that hospitals and health systems want to provide care for, but are not able to reach on their own.”
Hospital Roles in Building Community Partnerships
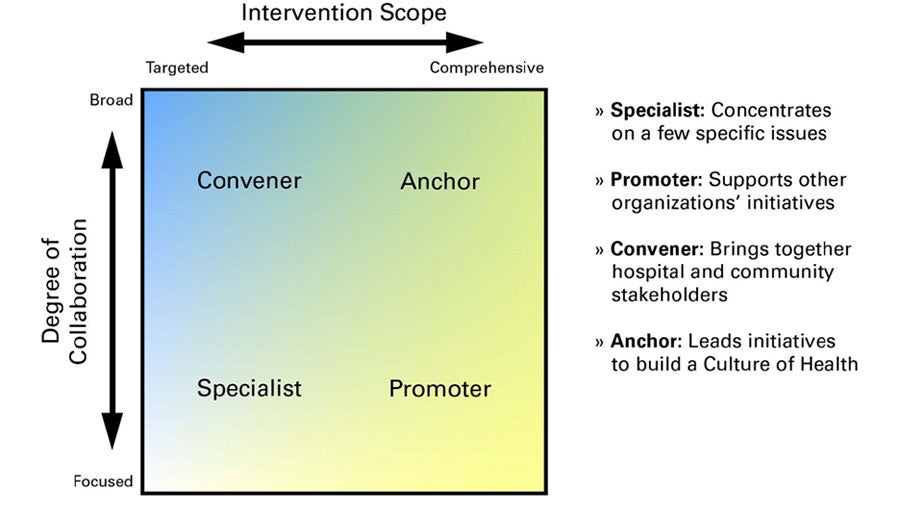
Source: Creating Effective Hospital-Community Partnerships to Build a Culture of Health,” Health Research & Educational Trust/American Hospital Association, 2016.
Bailey added that it’s important to look outward and acknowledge that improving a community’s health and wellness requires partnering with community leaders. Oftentimes, those leaders are not elected officials or individuals with titles, she said. Instead, they are the individuals that residents informally look to and respect for their wisdom and ability to speak on their behalf.
Leveraging Strengths
Bailey’s perspective is one that is not lost on Salem Health, a regional health system based in Salem, Oregon, which seeks partnerships that will leverage the strengths of everyone involved.
Leilani Slama, Salem Health’s chief communications and community relations officer, noted, “As a health system, we can’t always get close enough to a problem to impact it, and we want to support the types of organizations that can. Or we may see opportunities where combining our resources gets us much further than trying to muddle forward in silos.”
Despite a hospital’s or health system’s desire to improve community health, its primary purpose and focus have been to provide health care. “Our toolbox in health care has been limited,” said Dora Barilla, group vice president, community health investment, at Providence St. Joseph Health, a 51-hospital system based in Renton, Washington. “To drive a lot of the health outcomes and achieve the health goals that we want, we need to have authentic partnerships in our community. We have a housing ministry within Providence and continue to focus on social conditions, but that’s not our main course of business. We have to partner and align with other sectors.”
To strengthen community trust in health care organizations, Bailey believes that a partnership must be more than transactional. It must be a long-term investment in a reciprocal relationship in which all partners have a meaningful role in an initiative — its planning and solutions. The best role for hospitals and health systems is not always to be the leader. As Barilla observed, hospitals and health systems can be a catalyst, provide support services like data analysis and advocacy, or supply other needed resources and infrastructure.
Impact of Social Needs
COVID-19 has brought the impact of social determinants of health into even sharper focus. The pandemic has disproportionately affected racial and ethnic minorities in large part because their general health has been disproportionately affected by socioeconomic factors. The impact further heightens feelings of distrust that marginalized populations may have for some institutions, including hospitals and health systems.
Slama voiced the need and opportunity for developing partnerships to address the community’s health disparities, noting that Salem Health is focused not only on identifying the demographic and socioeconomic factors contributing to the county’s high rate of COVID-19 infection but also on answering the question, “What can we do to change it?” Slama explained: “We can’t do this without partnerships. We need to better understand and partner with others in the community to strengthen our cultural competency. Our traditional channels of communication, like public service announcements on radio, aren’t getting to the populations we need to reach. This is an opportune time for reflection and understanding about how to do things differently.”
Improving the health of the community overall will require all sectors, not just health care, to think more holistically. As Barilla posed it: “What role would the hospital or health system play? What role would housing play? What role would education play?” Both Bailey and Barilla advised that hospitals and health systems look broadly to build new partnerships, ensuring they are reaching all populations in their communities, not just the ones that seek care at their organizations.
To overcome the legacy of distrust, Bailey underscored the importance of approaching community partnerships with curiosity and interest and not assuming your organization has the definitive answer. Instead, the aim should be empowering those who live and work in the community to help identify the issues and give voice to the message. “People are tired of being told something is wrong with them,” Bailey noted, adding that hospitals and health systems can be more successful when they build on community leaders’ strengths to “lift people and their communities up, not to fix them.”
Just Show Up
Developing relationships in the community also is important. Slama shared that Salem Health’s partnerships have evolved over time. Hospital representatives began by “showing up at the table” without any assumptions or problems for the group to solve. Instead, it was enough to just start a conversation to better understand an issue. “We may engage actively in a partnership, or we may just lend our support and advocacy. It is starting with the relationships,” she said. “When you build the relationship, you have a better understanding of how the hospital or health system can support or contribute as opposed to coming to the table saying, ‘We’re here to solve it.’ We want to be viewed as a community hospital that is there for the community.”
“Engaging with stakeholders is the only way we can really understand why people make certain decisions or take certain actions,” Slama observed. “Oftentimes, the stakeholder you hadn’t thought of gives you the best insights.”
Slama shared an example of a partnership created to address adolescent mental health. The partners thought they had included every community stakeholder that touched teens in some way, but parents and teens were initially overlooked as key stakeholders. When the group recognized that these key stakeholders were not comfortable talking about suicide, Salem Health and the school district implemented listening sessions in the schools to hear from students and parents. Only then was the partnership able to set goals and act, Slama said.
Who Is Better Positioned To Do Something?
Hospital and health system boards can be catalysts for successful community partnerships in a number of ways including:
- Promote a culture of inclusion that focuses on health equity throughout the organization, beginning with the board. Work toward a board composition that accurately reflects the communities served in terms of race, ethnicity, gender and age.
- Actively participate in the community health needs assessment and ensure that areas identified as priorities are reflected in organizational strategies, goals and budget.
- Promote and support the development of community partnerships that are focused on shared goals and objectives, and leverage resources for maximum impact.
- Regularly monitor community partnerships to evaluate progress against mutually agreed upon goals.
- Communicate the efforts and results of these partnerships to increase transparency and build trust.
Trustee Takeaways
- Are your hospital’s/health system’s community partnerships well aligned with your strategic priorities?
- What roles have your community partnerships played in advancing your strategic aims?
- Does your board’s composition reflect the racial and ethnic profile of your community?
- Are your partnerships transactional or long-term investments designed to build on the strengths of leaders in the community?
- How are board members and executives active in key sectors of the community?
- What steps can your board take to support strong partnerships with others in your community?
The Salem Health governing board recently made a seemingly counterintuitive decision, but one designed to advance community benefit and community partnerships. The board eliminated its community benefit committee and shifted the work to the board’s planning committee. The decision reflects the three- to five-year commitment required to move the needle on population health. It also reflects the engagement and work of the board in identifying the organization’s population health strategy, how Salem Health identifies the community’s various populations, and the need to prioritize problems that require the greatest focus. The change also gives the board greater oversight in ensuring that the strategic plan is actually improving community health. Overall, the committee change reflects the board’s recognition that there are influences that Salem Health may not be able to directly affect, but which significantly affect residents’ health and the care they need from the health organization.
Barilla emphasized the need for board members to be a bridge to the community. Both she and Slama stressed the need and benefit of having board members and health system executives participate on the boards of local food banks, housing organizations and other local nonprofits.
“Who is better positioned to do that than our board members?” asked Barilla. “They hear what’s happening in the community and are a voice of education to the organization about what the community needs. They can be that bridge and liaison to a better outcome overall. They can ask the right questions, encourage resource allocation and hold the health system accountable to the common visions and outcomes that we all want to achieve. If we have boards playing the right role, I really believe they can transform the health of their communities.”
Erica M. Osborne (eosborne@viahcc.com) is a principal with Via Healthcare Consulting and based in Carlsbad, California. Cindy Fineran (cfineran@viahcc.com) is a senior consultant with Via Healthcare Consulting and based in Salem, Oregon.
Please note that the views of the authors do not always reflect the views of the AHA.
