Affordability
Understanding Affordability and Value in Health Care
Hospitals and systems can help reconcile differing perspectives
By Priya Bathija
Affordability is one of the most important challenges influencing Americans’ ability to access health care.[1] However, no single, agreed-upon definition of health care affordability exists because it is influenced by many complex factors.
Trustee Talking Points
- Affordability must be discussed in the context of value.
- Value, however, can mean different things to different people.
- Hospitals and systems must consider the needs and wants of patients.
- A common understanding of value can lead to changes that reduce costs.
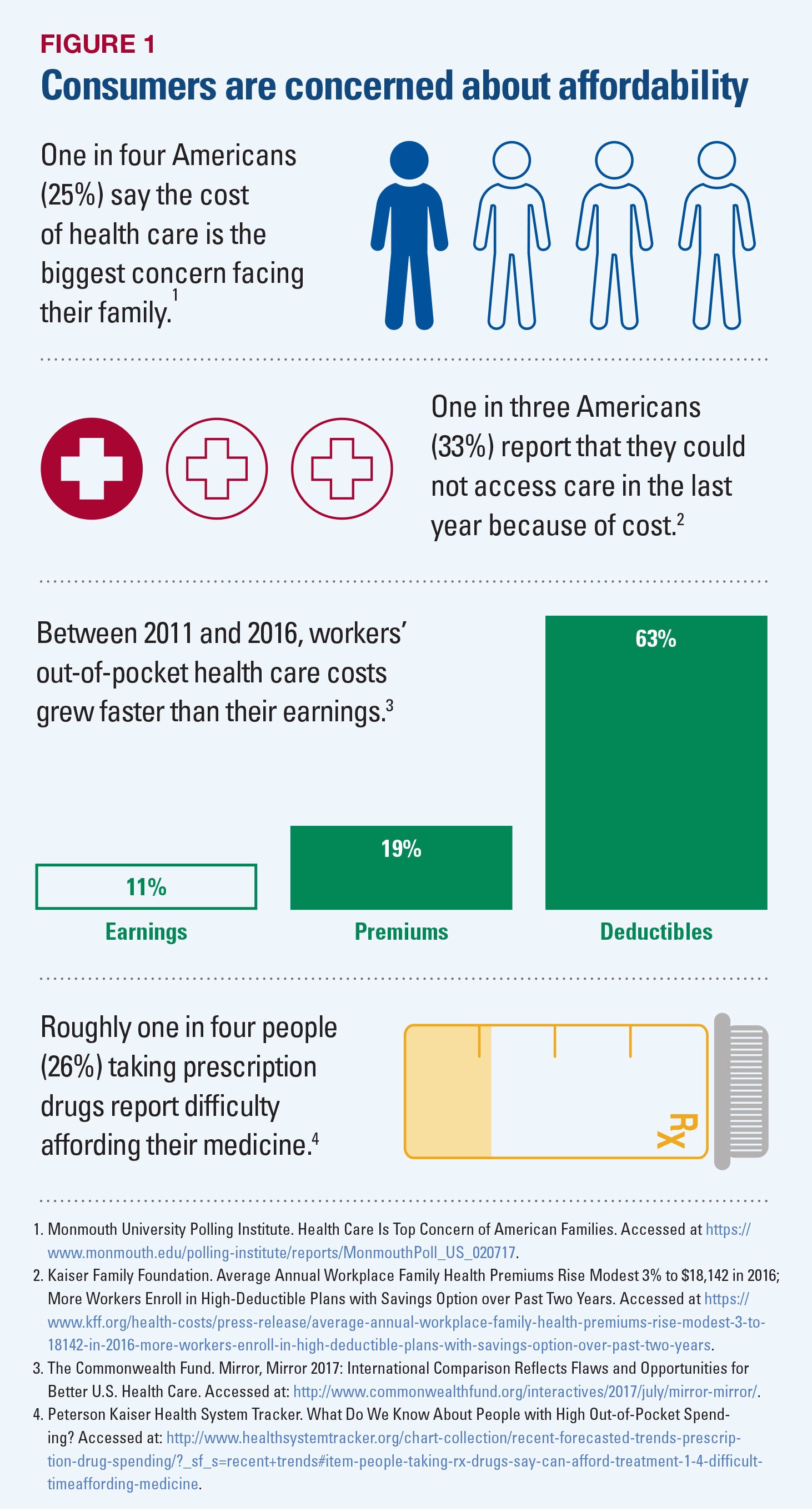
Affordability also is of increasing concern for many citizens. Individuals and families report difficulty paying for health care services and prescription drugs, as depicted in Figure 1.
Meanwhile, employers are anxious about their increasing contributions to employee health plans. In addition, federal and state governments are troubled by rising per capita spending on health care, growing budget deficits, and which priorities to fund, such as Medicare and Medicaid, education or infrastructure.
A Broader Context
While affordability is highly subjective and means different things to different consumers, patients, employers, government, providers and payers, “affordable health care” is often viewed generally as an issue of the cost of care. Yet, discussing affordability solely in terms of cost provides an incomplete picture that fails to consider the level of access and quality of care received for each dollar spent. With this in mind, AHA considers affordability though the lens of value.
There has been significant interest in and discussion around what value in health care delivery means; however, there is no agreed-upon definition or expectation of value across the health care field. Perspectives vary widely, are at times inconsistent and, in many instances, do not align among consumers, employers, payers, health care providers, policymakers, and community partners.
Hospitals and health systems, for example, offer greater value to individual consumers by investing in strategies that lower costs, improve quality and enhance the patient experience of care. These strategies include, among other things, coordinating care, reducing clinical and operational variation, addressing the social determinants of health, and managing the health of the populations they serve — all of which are occurring in a fragmented payment landscape.
Health care payers, including insurers, employers, and governmental programs, are continuing to transition from fee-for-service to value-based payment methodologies, which are intended to support and incentivize many of the strategies deployed by hospitals and health systems described above. For example, the Department of Health and Human Services intends to shift the majority of Medicare payments away from fee-for-service and toward quality and value by the end of 2018.[3]
For individual consumers, the definition of value is very personal. For some, value is simply finding the right mix of health care services to meet their needs. Some only want the best there is to offer, regardless of price or convenience. Yet others focus solely on price, typically the price of front-end premiums, to determine whether the health care services offered will match their budgets.
These differing perspectives make it difficult to land on one common definition of value in the context of health care delivery. And, without a consistent definition, it is challenging to improve and enhance value across the field.
Toward a Common Understanding of Value
In 2006, Harvard Business School Professor Michael Porter offered the most commonly used definition of value for the health care field: health outcomes achieved per dollar spent.[4] Others in the health care field have adopted this working definition. And, generally speaking, there is a consensus that value resides at the intersection of an individual consumer’s perception of the quality of a good or service and the amount he or she is willing to pay for it.[5]
While a starting point, this definition points to one of the true challenges in defining value: it means different things to different people. In their work on this issue, the Healthcare Financial Management Association (HFMA) set forth four factors that expand upon this definition and influence an individual’s concept of value: access, safety, respect and outcomes. The HFMA explained that consumers want access to affordable health care.[6] Once they have access, they assume that their care will be delivered in a safe manner and that their health care providers will respect their needs and desires. They also expect that the care will lead to outcomes that make them feel better and function at their desired level.[7]
Even with this working definition of value, it is extremely hard to hone in on exactly what value means at a practical level in health care. In 2017, the AHA held a series of conversations with hospital and health system leaders to discuss the issue of health care affordability and the role hospitals and health systems play in addressing rising health care costs. As part of those conversations, the AHA asked its membership whether the association should consider affordability through the lens of value. AHA members clearly indicated that value must be at the forefront as the hospital field addresses affordability.
Trustee Takeaways
Boards can ask the following questions to enhance their understanding of affordability and value in health care:
- Who are our organization's key stakeholders (e.g., patients, their families, employers, etc.), and what do affordability and value mean to them?
- How is our organization continuing to monitor what affordability and value mean to those we serve?
- What steps has our organization taken to address stakeholders' needs related to health care affordability and value?
- How should our board keep apprised of our organization's efforts to continue to improve the affordability and value of the health care we deliver?
The AHA membership agreed that value is directly linked to an individual’s personal experiences and perspectives. Life circumstances, including age, health status, cultural influences, or simply one’s proximity to health care services in their community, can have a significant impact on an individual’s definition of value. And, while patient experience is subjective, hospitals and health systems must consider the needs and wants of patients as they move forward in the quest to enhance value.
Members also indicated that we must consider the full story when looking at value, including not only the cost of care, but also patient experiences and outcomes. In other words, they do not view value as simply a code word for cost reduction. They view it as an opportunity to redesign the delivery system, improve quality and outcomes, manage risk and offer new payment models, and implement operational solutions that will reduce costs.
Based on this feedback, as the AHA works to address the issue of value, it will use the following definition:
Value = Outcomes & Patient Experiences/Cost
The AHA also has launched The Value Initiative to provide members with a variety of tools and resources to address health care affordability and value. For example, the “Members in Action” case studies offer real-world examples of hospitals and health systems implementing changes that promote value by reducing costs, improving quality and enhancing the patient experience.
While there are certainly challenges in defining affordability and value and each piece of the value equation, hospitals and health systems remain committed to delivering on this equation and providing leadership for the health care field.
Author’s note: This article is based on two resources from The Value Initiative: “Issue Brief 1: Framing the Issue of Affordable Health Care” and “Issue Brief 2: What Does Value Mean?” For more on these issue briefs, which include sources for further reading as well as additional resources on the issues of affordability and value, visit www.aha.org/TheValueInitiative.
Priya Bathija (pbathija@aha.org) is vice president of The Value Initiative at the American Hospital Association.
Endnotes:
1. Health Affairs. Affordability: The Most Urgent Health Reform Issue For Ordinary Americans. Accessed at: https://www.healthaffairs.org/do/10.1377/hblog20160229.053330/full/.
2. Bureau of Labor Statistics. Household Healthcare Spending in 2014. Accessed at: https://www.bls.gov/opub/btn/volume-5/household-healthcare-spending-in-2014.htm.
3. New England Journal of Medicine. Setting Value-Based Payment Goals — HHS Efforts to Improve U.S. Health Care. Accessed at: http://www.nejm.org/doi/full/10.1056/NEJMp1500445.
4. Harvard Business Review. The Strategy That Will Fix Health Care. Accessed at: https://hbr.org/2013/10/the-strategy-that-will-fix-health-care.
5. HFMA’s Value Project. Value in Health Care: Current State and Future Directions. Accessed at: http://www.hfma.org/Content.aspx?id=1126.
6. Id.
7. Id.