New Delivery Models
Creating Age-Friendly Health Systems
An innovative model addresses the unique care needs of older adults
by Marie Cleary-Fishman, Jay Bhatt and Jonathan R. McKinney
The nation’s adult population over age 65 is projected to reach 83.7 million by the year 2050, an increase from 21% of the population in 2012 to more than 39% in 2050. This population has unique and complex health care needs, which makes medical care more challenging and complicated. Some challenges that persist: transitions between care settings; side effects and adverse drug interactions from multiple medications; lack of care planning that incorporates culture, values and goals of the patients and their families; communication barriers due to language and hearing; and changing care preferences that favor older adults remaining independent and in their home.
Many older adults also face challenges with change in self-identity; social isolation and loneliness; decreased mobility; loss of independence; and change in resources, including food and financial insecurity. These factors call for innovative care delivery models that respond to patients’ personal preferences, medical needs and values. An age-friendly health system could be the key approach to this need.
An Innovative Health Care Model for Older Adults
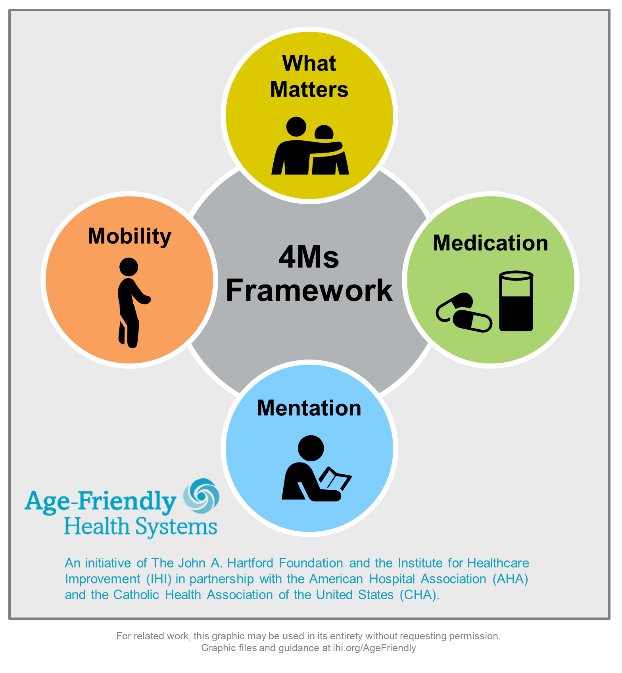
Age-Friendly Health Systems is an initiative of the John A. Hartford Foundation and the Institute for Healthcare Improvement in partnership with the American Hospital Association and the Catholic Health Association of the United States. The initiative is designed to meet the needs of older adults, looking beyond acute events, engaging the whole community and achieving better health for older adults.
Age-Friendly Health Systems is an evidence-based model to support the needs of the aging community by focusing on four key areas: what matters, medications, mobility and mentation — better known as the 4Ms Framework. Through this initiative, we aim to improve patient care, safety and outcomes; improve patient and family engagement in care; and reduce outcomes such as length of stay and readmissions.
The 4Ms Model
This ideal health care system for aging Americans boils down to the 4Ms model where the M’s are considered and addressed together, all the time:
- What Matters: Know and align care with each older adult’s specific health outcome goals and care preferences including, but not limited to, end-of-life care, and across settings of care.
- Medications: If medications are necessary, use age-friendly medications that do not interfere with What Matters, Mentation or Mobility.
- Mentation: Prevent, identify, treat and manage depression, dementia and delirium across settings of care.
- Mobility: Ensure that older adults move safely every day in order to maintain function and to do What Matters.
4M Action Steps
- What Matters:
- Educating care providers on appropriate conversations with patients who have a serious illness; addressing patients’ concerns and goals.
- Involving an interdisciplinary team to meet and discuss complicated cases and implement new ideas generated by these discussions.
- Medications:
- Scheduling pharmacovigilance meetings among care providers to ensure patient safety.
- Redesigning medication reconciliation processes.
- Mentation:
- Reaching out to inpatient providers to help ensure delirium notification and results are communicated and understood.
- Studying the impact of dementia on illness presentation.
- Mobility:
- Developing a primary care model focused on mobility as a lever for fall risk management.
- Increasing frequency of 1:1 ambulation with patients.
Age-Friendly Health Systems elevate traditional models of care for older adults and their caregivers in ways that preserve dignity and encourage independence. An effective age-friendly health system means: older adults get the best care possible; health care-related patient safety incidents approach zero; and patient experience and value are optimized for all — patients, families, caregivers, health care providers and health systems.
Becoming an Age-Friendly Health System: A Case Example
Care New England (CNE) realized to do true population health, it needed to meet the needs of its older adults, particularly at Kent Hospital in Warwick, Rhode Island, where the patient volume is the highest. A needs assessment at Kent Hospital showed that 30% of hospital admissions were patients over the age of 65, and of that group, most were over 85. Since 2014, the health system and Kent leadership teams have supported the growth of a service line in geriatrics and clinical programs to serve the needs of older adults across the continuum of care.
CNE’s participation in the Age-Friendly Health Systems initiative focused on building an Acute Care for Elders (ACE) unit at Kent Hospital. At the baseline, many seeds were in place to drive success: Leaders fully supported a mission-driven focus to improve care of older adults; a two-year effort on creating delirium prevention and management protocols had just kicked off; and pharmacy teams had begun working on eliminating potentially inappropriate medications.
The team’s aim was to set up the new geriatric unit using the 4Ms model — what matters, medication, mentation and mobility — and focus on 1) documenting “what matters most” and 2) implementing delirium screening and a prevention power plan for all patients admitted to the 10-bed unit. The health system spent just over a year planning and working toward converting an existing hospital unit to serve as the new 10-bed ACE unit.
In the ACE unit, each patient is reviewed during typical hospital rounds, and then each of the 4Ms is reviewed to round out the day’s plan and the care plan overall. The geriatrics team uses the 4Ms to organize recommendations for each patient on the unit, as well as across the hospital on the geriatrics consultation service.
The health care team uses a dashboard to track the ACE unit outcomes and key performance metrics. Since opening the unit in February 2019, Kent Hospital has served, on average, 76 patients per month with an average age of 86. Length of stay each month has decreased as have patient falls. Staff and patient and family satisfaction has risen tremendously. Kent intends to expand the size of the ACE unit to 20 beds.
Since implementing the 4Ms model on Kent’s ACE unit, CNE has begun using the model to frame and organize recommendations on all geriatric consultations hospitalwide. The health system also is enrolling an ambulatory practice to spread the Age-Friendly Health Systems model further. In addition, CNE is beginning to collaborate with its emergency department physician and nursing leaders to implement the 4Ms model for older adults in the ED. Hospital and health system leadership support making the older adult work a high priority and part of is executive action plan.
How Can Trustees Be Involved?
Hospitals and health systems have developed governance committees to review and provide strategic guidance on moving quality forward. It is important for trustees to play a critical role in providing guidance, raising questions and moving forward an age-friendly health system — one that will care for them someday.
We encourage hospitals and health systems to join us in deploying the 4Ms Framework and embracing age-friendly care. The benefits of joining this movement include:
- Redeploying and prioritizing existing hospital/health system resources.
- Supporting your health organization’s mission, vision and values.
- Putting your organization ahead of the curve in preparing for the impending market shift.
- Achieving “Age-Friendly Health System Participant” or “Committed to Care Excellence” recognition.
Age-Friendly Recognition
The first AHA Age-Friendly Health Systems action community concluded in early April, with 75 teams achieving “age-friendly” recognition. This cohort of 184 health care teams and 12 allied associations worked simultaneously to implement the 4Ms and provide high-quality care that meets the unique needs of older adults. One care team participating designed a telehealth visit template that includes the 4Ms and is used through a virtual telehealth clinic. At another participating organization, nursing staff are spending time digging deep into the 4Ms, which is improving patient satisfaction and the discharge process.
The AHA will be hosting another Age-Friendly Health Systems action community in fall 2020.
To get involved, email AFHS@aha.org. You can learn more about the initiative and action community at AHA.org/age-friendly.
Marie Cleary–Fishman (mfishman@aha.org) is vice president, clinical quality, at the American Hospital Association. Jay Bhatt, D.O., (jay@drjaybhatt.com) is a practicing internist and former chief medical officer at the American Hospital Association. Jonathan R. McKinney (jmckinney@aha.org) is director, office of the CMO and operations, at the American Hospital Association.
Please note that the views of the authors do not always reflect the views of the AHA.