
Health Equity
The Board’s Role in Advancing Healthier, More Equitable Communities
Strategies and collaboration to improve health equity
By Anne Rooney and Barbara Lorsbach
The sobering fact of health inequity has been spotlighted through the recent experiences with coronavirus infections and racial injustice in the United States. As a result, boards and senior health care leaders are deepening their commitment to advancing health equity. The path forward has significant implications that are important for trustees to understand.
Understanding Health Equity
Twenty years ago, the Institute of Medicine urged a call to action to improve the American health care system. Its influential report, Crossing the Quality Chasm: A New Health System for the 21st Century, addressed six key dimensions in which our overall health care system functioned at lower levels than it should. The report’s aims for improvement stressed that quality health care should be safe, effective, patient centered, timely, efficient and equitable. Although considerable progress has been made in most of these quality dimensions over the past two decades, the sixth dimension — equitable (or equity) — has shown little improvement.
Health equity is defined as everyone having a fair and just opportunity to be as healthy as possible. In the U.S. each year, millions of people experience food insecurity, homelessness or an inability to access medical care. For older adults on fixed incomes, the high price of prescription drugs may make it difficult for them to access needed medications. Families may lack health insurance or the ability to navigate the health system due to language and cultural barriers. Some people in our country live in “food deserts,” areas with limited availability of fresh fruits and vegetables. Social isolation and housing in areas where violence has become a regular occurrence also affect overall health. Some of these problems “hide in plain sight” — even in affluent communities.
Health Inequity and COVID-19
Data from the U.S. Centers for Disease Control and Prevention reveal that COVID-19 disproportionately affects Black and Latino people, with infection rates nearly three times the rates for their white neighbors. Older adults have substantially higher infection and death rates. These disparities are widespread across the U.S., throughout urban, suburban and rural areas.
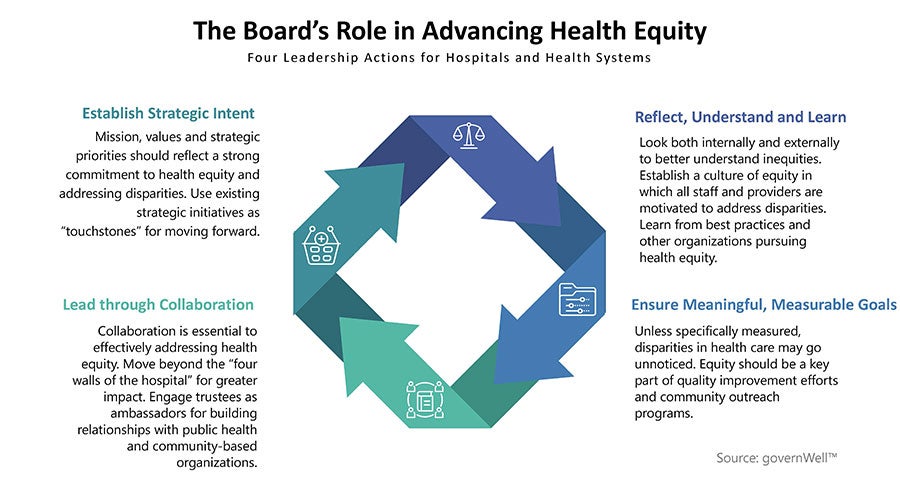
Source: The governWell BoardBrief on Health Equity, 2020. Infographic used with permission.
Experts cite many possible reasons for disparities, including social determinants of health, defined as the nonmedical factors that influence health outcomes. They are the circumstances in which people are born, grow up, live, work and age, and the systems shaping conditions of daily life. Examples of social determinants that have increased coronavirus infection rates include multigenerational or crowded housing, food insecurity, lack of health insurance, essential jobs that cannot be done remotely and use of public transportation. Research demonstrates that up to 80% of health outcomes are driven by these social determinants.
Establishing Strategic Intent
How does the board promote and advance health equity? Boards, senior executives and clinical leaders set the strategic foundation for the organization through the mission, values and strategic priorities. Boards also play a critical role in ensuring that health equity is in some way addressed, with defined improvement actions and metrics to measure progress. Specific approaches will vary greatly depending on the hospital or health system and the needs of their communities.
An excellent place to start is with the community health needs assessment that many hospitals conduct every three years. Hospitals also use tools, such as the County Health Rankings and Roadmaps, to assist them in understanding the disparities in their community. Information on a wide spectrum of variables — such as racial, ethnic, education and language demographics of the community — along with data on other factors — such as average life expectancy; chronic disease rates; and levels of poverty, food insecurity and unemployment — will help the hospital identify the most urgent unmet needs in the community.
Another strategy to advance health equity is the #123forEquity Pledge to Act to eliminate health disparities — an initiative of the American Hospital Association. More than 1,600 hospitals and health systems have taken the pledge to work to accelerate achieving four areas of improvement: increasing the collection and use of race, ethnicity and language preference data; increasing cultural competency training; increasing diversity in governance and leadership; and improving community partnerships.
Even the most well-intentioned efforts to advance health equity are less likely to succeed if those efforts are not part of a broader culture of equity. When leadership and staff recognize that disparities exist within the organization and view inequality as an injustice that must be redressed, that organization has a strong culture of advancing health equity.
Ensuring Meaningful, Measurable Goals
Although it will be up to senior management and clinical leaders to ensure that the strategic activities are implemented in practice, the board is responsible for seeing that the plans are being followed. Metrics should be established in advance to evaluate progress toward goals. These performance data should be reported to the board or its designated committees at defined intervals, such as quarterly. Data that the board will want to monitor will depend on the specific improvement initiatives that are underway, and should have enough specificity to identify trends and gaps.
Leading Through Collaboration
Individual hospitals and health systems cannot independently do everything that is needed to fulfill their mission commitment to the community and health equity. Thinking independently fails to leverage the opportunities that come with joint efforts and to move beyond the four walls of the hospital. Potential partnership opportunities include working with county or city health departments, food pantries, homeless shelters, faith communities, and civic and social service organizations. Some smaller organizations have strong missions; however, they may need resources to fully achieve their potential. By simply supporting these organizations with expertise that already exists within hospitals and health systems, they can have a greater impact on communities. Developing and governing successful community partnerships require high levels of trust and the ability to envision a future where health and health care look different and are better than today.
Inequity in our health system remains a major public health and societal challenge. As community representatives and fiduciary stewards, hospital and health system board members play a critical role in prioritizing, understanding, monitoring and collaborating to improve health equity. Board leadership is critical to advancing healthier, more equitable communities.
Anne Rooney, RN, MS, MPH, (annelrooney14@gmail.com) is an advisor of governWell and president of Anne Rooney and Associates Inc. Barbara Lorsbach, FACHE, (blorsbach@governwell.net) is president of governWell. Both are based in Oak Brook, Illinois.
Please note that the views of authors do not always reflect the views of the AHA.
